It began with a three-and-a-half line email, sent cold, over Columbus Day weekend 2020.
That message, sent to Conway School of Nursing (CSON) Dean Emerita Patricia McMullen, ultimately resulted in a $5 million gift to the Conway School from the Institute for Technology in Health Care (ITHC) in honor of its founder, Dr. Cesar Caceres.
The gift, to be made over the course of five years, will establish the state-of-the-art Cesar A. Caceres Simulation Center in the new nursing and sciences building that is currently under construction, and will help Conway School faculty prepare students for some of the many scenarios they will face during their nursing careers.

“[This gift] will allow us to construct not just a cutting-edge simulation center, but one that is visionary and will serve to educate nurses and other healthcare providers for many years to come.”
— Patricia McMullen, dean emerita of the Conway School of Nursing
Who was Dr. Caceres?
Born in Honduras in 1927, Cesar Caceres was the son of the Honduran ambassador to the United States. According to Dr. William Ayers, president of the ITHC board, Caceres grew up in D.C. and was an internist and cardiologist who earned his degrees at Georgetown University. The two met in the late 1960s when Ayers was assigned to Caceres’ lab at the U.S. Public Health Service. Caceres and those in his lab, the Medical Systems Development Laboratory, were part of a government program tasked to find ways to help prevent heart disease.

“Prevention at that time meant screening large numbers of people,” Ayers said. “They thought that automating the electrocardiogram for screening was the thing to do, so our focus was to get computer recognition of the electrocardiogram for purposes of mass screening to prevent heart disease. Dr. Caceres thought we could do it.”
“In my opinion, Dr. Caceres’ contributions have been underappreciated and relatively unknown. One of my interests on the board was to rectify that through a naming opportunity, something in perpetuity with an overlap of mission.”
— Dr. William Ayers, president of the ITHC board
No one had ever shown the feasibility of it before, but the collection of electrical engineers, computer programmers — in the 1960s, essentially math majors, Ayers said — and “eager-beaver cardiologists, of which I was one,” joined forces to see if there was a way to make existing electrocardiograph machines talk to computers.
“Cesar said, if you’re going to put computers into medicine, you don’t change medicine. In other words, don’t build a new EKG machine, use what’s out there and make it work.”
The group programmed the computer to measure intervals and amplitudes, discern pattern recognition, and analyze the wave that came out of the EKG machine. “It was sort of very primitive — by today's standards — artificial intelligence,” Ayers said. “Dr. Caceres showed it could be done.” After taking it through beta testing with groups that included IBM, Digital Equipment Corporation, and EKG machine manufacturers, Dr. Caceres appeared before a health appropriations committee and demonstrated the computer-interpreted EKG.
“The guys in Congress asked him only one consequential question,” Ayers recalled. “They asked, ‘will this help my doctor in Pennsylvania?’ Basically, the answer was yes. If you go to your doctor today and have an electrocardiogram, they wheel in this machine and hook you up, the paper comes out, and it has a diagnosis. The fiducial software — measuring a point or line that is assumed as a fixed base for comparison — in that machine today comes from Dr. Caceres’ laboratory.”
The Public Health Service changed focus in the 1970s, and Caceres moved his lab to George Washington University (GW) in 1978, where the lab continued to work on how computers could be incorporated into medicine. “Our major focus was multiphasic health screening,” Ayers explained. “It’s not just the cardiogram, but a bunch of other medical signals that led to the formation of the automated medical record.”
Back to that email…
Dr. Caceres passed away in early February 2020, leaving no heirs. According to the terms of his will, his estate was liquidated, with the proceeds left to benefit the not-for-profit institute which supports organizations involved in technology in health care, HIV treatment, and clinical engineering. The seven-member, all-volunteer ITHC board was charged with finding organizations to support with these additional funds.
Then came the coronavirus pandemic.
The ranking of the Conway School of Nursing got the attention of Dr. Ayers.
“We had this large corpus of money, … but several of our usual grantees could not do their work because of the isolation brought on by the pandemic, and we couldn’t disperse enough money. Plus, we had more to give,” Ayers said.
It was his job as board president to find a solution. Then he remembered Carole “Pinky” Stone, the late wife of one of his best friends, Matthew. “She was a foundational member of the Catholic University nurse practitioner program,” he said. “I knew Carole — Pinky — and Catholic University, but at the time I didn’t know they were number five in the country in U.S. News & World Report for their online graduate degree program.”
The ranking got his attention.
“We realized how the mission of the nursing school in this area of simulation education in health care, not research, really fit our mission. All of those keywords are in there someplace: technology applied to healthcare,” he said.
And so he sent the email saying he had some ideas he wanted to share with McMullen. She and Ayers scheduled a lunch meeting.
“Dean McMullen immediately saw the overlap of our missions,“ Ayers said. “It was a very easy fit.”
Starting small
Ayers suggested the University apply for a small, starter ITHC grant to begin with.
The application came from Dr. Jeanne Moore, the director of the University’s graduate-level family nurse practitioner program and a nationally certified family nurse practitioner who holds a B.S. in Computer Science from the University of Virginia. She and nursing faculty members Dr. Elizabeth Hawkins-Walsh and Dr. Janet Selway, had previously developed a course training simulated patients in collaboration with Dr. James Hampton and Dr. Marietta Hedges, faculty in Benjamin T. Rome School of Music, Drama, and Art. Through the program, drama students could learn to act the part of patients who nursing students would then evaluate.
Moore had wanted to conduct remote site visits of nurse practitioner students for years because “with online students it’s not physically or financially possible to perform them in person. People were starting to use video conferencing, and I thought it was a great idea.”
Then the pandemic hit, and healthcare visits via video conferencing became commonplace.
“Telemedicine was one of the things we were into when we were at GW, and people weren’t buying it,” Ayers said. “Pre-pandemic, the technology was there, the system was there, but nobody needed to use it. Now, it's going to be one of the things that will hold over after the pandemic, hopefully.”

In late 2020, Moore applied for and received the grant from ITHC that provided equipment to help her students learn how to conduct telehealth visits. That grant, recently renewed for a third time, has enabled Moore to teach more students the ins and outs of telehealth using TytoCare medical exam kits that measure heart rates and have various attachments and a high-res camera to help practitioners look in a patient’s ears, nose, and throat.
“I’m very supportive of what she’s doing,” Ayers said. “Every physician I know is using telemedicine. With nurse practitioners and applications being done here at Catholic University, they use a lot of devices, sensors, that the patient can put to their heart and hear heart sounds, to their lungs and hear their lung sounds. Not just the pulse rate, not just the electrocardiogram, a bunch of stuff. That made the connection with us, with our institute, more obvious.”
McMullen said ITHC funded several other grants in support of simulation and technology, providing money for the use of remote ophthalmoscopes to assess nurse practitioner student competencies for our online students, funding various types of equipment in support of skills masteries, and advancing the University’s telehealth competencies.
“Once we had that established relationship funding Ms. Moore’s project, we began to explore ways we could expand what we were doing in that context,” Ayers continued. He thought it was a prime opportunity to honor Dr. Caceres.
“In my opinion, Dr. Caceres’ contributions have been underappreciated and relatively unknown. One of my interests on the board was to rectify that through a naming opportunity, something in perpetuity with an overlap of mission,” Ayers said, adding he went to the board with a list of funding opportunities provided by the University. “Once they got all the information on the school of nursing, it was obvious.”
Finding the obvious, big need
Several board members visited campus and toured the nursing facilities. It was apparent to Ayers and other ITHC board members who visited the Tersigni Simulation Center that it needed to be upgraded and expanded. They also met with students. “They were very impressive,” Ayers said. “As a practicing physician in this city, Catholic University nurses are always well-regarded.”
David Want, M.S.N. 2017, D.N.P. 2020, assistant clinical professor in the Conway School, director of simulation, and a nationally Certified Healthcare Simulation Educator, said COVID-19 magnified the need for a new simulation center and simulation-based learning.
“Simulation is essentially built off experiential learning theory. It provides a safe space to practice and learn and make mistakes without the risk of harming a patient. Students then transfer those skills to real-life patients,” he said. “It’s a tool that produces better nurses that results in better outcomes and healthier people.”
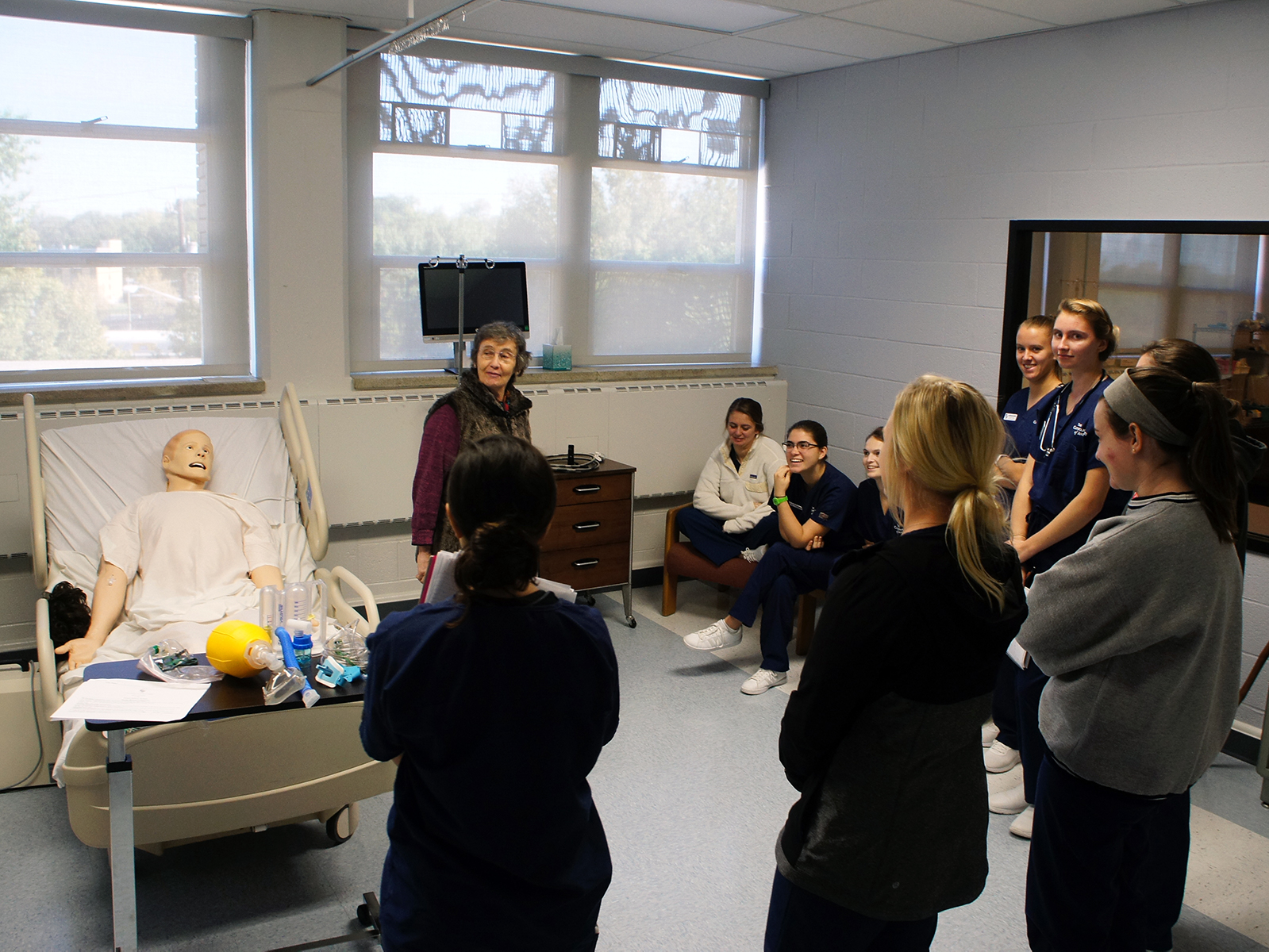
All undergraduate nursing students, about 150-200 per week, use the sim lab. What they learn there is applied to clinical scenarios that include conducting a health assessment or a physical exam, as well as working on their therapeutic communication skills. With tele-simulation, the formative learning experience shapes them.
Want said rapidly advancing technology has put constraints on the current physical space, but they also just need more room. “The barriers that we’ve run into are related to the need to expand beyond our current footprint.”
“The sim center is foundational. We really need it as soon as possible for teaching and for seeing students in life-like situations so we can gauge where they are in their learning.”
— Jeanne Moore, director of the Conway School of Nursing’s graduate-level family nurse practitioner program
Moore said most simulation centers at universities are “very different from what we have.”
“We can run sims simultaneously, but we only have two rooms that have examination tables,” she said, adding that “normal” sim centers often feature nurses stations, multiple exam rooms, waiting areas, as well as observation rooms where instructors can view their students without the students hearing or seeing faculty. “It feels very real. Students know they’ll be observed, but if they don’t feel the instructor’s presence or hear it, they’ll be more relaxed and natural.”
Hardware, such as added cameras and sound equipment, would enable faculty to record students during simulations from multiple angles. “We have basic equipment,” Want said, “but we can’t pan, or tilt, or zoom. Professors have to watch through a window, and students can hear us.”
The benefits of the Cesar A. Caceres Simulation Center
The new Cesar A. Caceres Simulation Center will not only increase the capacity available, but it will also alter the quality of the experience Catholic University can provide to its students, Want said.
“We’ll have four times the space we have now,” he added. “Each high-fidelity room could run a different experience, either with a simulated patient or with an actor.”
The new Caceres Center will include a debriefing room to review student performance during simulations and a simulated recovery room. The high-fidelity patient rooms will more closely mimic spaces in an acute care facility. In the building’s virtual reality suite, students either wear virtual reality goggles, or they work in an augmented reality setting, where the walls have various scenes projected upon them.
“All things we can’t do in our current space,” Want said.
From an instructor’s standpoint, Moore said simulation also allows professors to teach students about scenarios that are more rare.
“We can hold simulations about patients with psychiatric disorders, or provide a safe environment where a nurse can learn how to deliver bad news,” she said.
Thanks to the ITHC gift, a large portion of the second floor of the new nursing and sciences center will become the new simulation center. It will allow CSON faculty to expand available opportunities for simulation, as well as better integrate those experiences across all levels of curricula, rather than trying to cram everything into one semester.
“We’ll have four times the space we have now. Each high-fidelity room could run a different experience, either with a simulated patient or with an actor.”
—David Want, M.S.N. 2017, D.N.P. 2020, assistant clinical professor and director of simulation for the Conway School of Nursing
“The sim center is foundational. We really need it as soon as possible,” Moore said, “for teaching and for seeing students in life-like situations so we can gauge where they are in their learning.”
Just as the new building will help attract additional students, Want said he hopes the Cesar A. Caceres Simulation Center will also help attract more faculty and staff to the Conway School to help expand its programming.
“Schools with a similarly sized simulation center will have between eight and 16,” he said, adding while he’s the only dedicated faculty member who teaches in the Tersigni Center full time, two more are joining him in the fall. “ITHC’s gift will enable all the times we’ve talked about.”
McMullen called the ITHC grant “seminal.”
“It will allow us to construct not just a cutting-edge simulation center, but one that is visionary and will serve to educate nurses and other healthcare providers for many years to come,” McMullen said.
Published on: Wednesday, June 8, 2022
Campaign Theme: Academic Environment
Division:
Tags: Nurse Practitioner, Simulation Lab, Caceres, Conway





